Accommodative Dysfunction
|
Focusing problem that is unrelated to aging
changes in the lens of the eye.
|
Amblyopia
|
Lazy eye, or amblyopia, is the loss or lack of
development of central vision in one eye that is unrelated to any eye
health problem and is not correctable with lenses. It can result from a
failure to use both eyes together. Lazy eye is often associated with
crossed-eyes or a large difference in the degree of nearsightedness or
farsightedness between the two eyes. It usually develops before the age
of 6, and it does not affect side vision.
Symptoms may include noticeably favouring one eye or
a tendency to bump into objects on one side. Symptoms are not always
obvious.
Treatment for lazy eye may include a combination of
prescription lenses, prisms, vision therapy and eye patching. Vision
therapy teaches the two eyes how to work together, which helps prevent
lazy eye from reoccurring.
Early diagnosis increases the chance for a complete
recovery. This is one reason why the American Optometry Association
recommends that children have a comprehensive optometry examination by
the age of 6 months and again at age 3. Lazy eye will not go away on its
own. If not diagnosed until the pre-teen, teen or adult years, treatment
takes longer and is often less effective.

Early diagnosis increases the chance for a complete recovery. |
Astigmatism
|
Astigmatism is a vision condition that causes
blurred vision due either to the irregular shape of the cornea, the
clear front cover of the eye, or sometimes the curvature of the lens
inside the eye. An irregular shaped cornea or lens prevents light from
focusing properly on the retina, the light sensitive surface at the back
of the eye. As a result, vision becomes blurred at any distance.
Astigmatism is a very common vision condition. Most
people have some degree of astigmatism. Slight amounts of astigmatism
usually don’t affect vision and don’t require treatment. However, larger
amounts cause distorted or blurred vision, eye discomfort and headaches.
Astigmatism frequently occurs with other vision
conditions like nearsightedness (myopia) and farsightedness (hyperopia).
Together these vision conditions are referred to as refractive errors
because they affect how the eyes bend or “refract” light.
The specific cause of astigmatism is unknown. It
can be hereditary and is usually present from birth. It can change as a
child grows and may decrease or worsen over time.
A comprehensive optometric examination will include
testing for astigmatism. Depending on the amount present, your
optometrist can provide eyeglasses or contact lenses that correct the
astigmatism by altering the way light enters your eyes.
Another option for treating astigmatism uses a
corneal modification procedure called orthokeratology (ortho-k). It is a
painless, non-invasive procedure that involves wearing a series of
specially designed rigid contact lenses to gradually reshape the
curvature of the cornea.
Laser
surgery is also a possible treatment option for some types of
astigmatism. It changes the shape of the cornea by removing a small
amount of eye tissue. This is done using a highly focused laser beam on
the surface of the eye.
What causes astigmatism?

When the cornea or lens of an eye is irregularly shaped, vision may be
out of focus at any distance.
Astigmatism occurs due to the irregular shape of
the cornea or the lens inside the eye. The cornea and lens are primarily
responsible for properly focusing light entering your eyes allowing you
to see things clearly.
The curvature of the cornea and lens causes light
entering the eye to be bent in order to focus it precisely on the retina
at the back of the eye. In astigmatism, the surface of the cornea or
lens has a somewhat different curvature in one direction than another.
In the case of the cornea, instead of having a round shape like a
basketball, the surface of the cornea is more like a football. As a
result, the eye is unable to focus light rays to a single point causing
vision to be out of focus at any distance.
Sometimes astigmatism may develop following an eye
injury or eye surgery. There is also a relatively rare condition called
keratoconus where the
cornea becomes progressively thinner and cone shaped. This results in a
large amount of astigmatism resulting in poor vision that cannot be
clearly corrected with spectacles. Keratoconus usually requires contact
lenses for clear vision, and it may eventually progress to a point where
a corneal transplant is necessary.
How is astigmatism diagnosed?

A phoropter and a retinoscope are instruments commonly used by
optometrists to measure refraction.
Astigmatism can be diagnosed through a
comprehensive eye examination.
Testing for astigmatism measures how the eyes focus light and determines
the power of any optical lenses needed to compensate for reduced vision.
This examination may include:
Visual acuity – As part of the testing, you’ll be
asked to read letters on a distance chart. This test measures visual
acuity, which is written as a fraction such as 20/40. The top number is
the standard distance at which testing is done, twenty feet. The bottom
number is the smallest letter size you were able to read. A person with
20/40 visual acuity would have to get within 20 feet of a letter that
should be seen at forty feet in order to see it clearly. Normal distance
visual acuity is 20/20.
Keratometry – A keratometer is the primary
instrument used to measure the curvature of the cornea. By focusing a
circle of light on the cornea and measuring its reflection, it is
possible to determine the exact curvature of the cornea’s surface. This
measurement is particularly critical in determining the proper fit for
contact lenses. A more sophisticated procedure called corneal topography
may be performed in some cases to provide even more detail of the shape
of the cornea.
Refraction – Using an instrument called a
phoropter, your optometrist places a series of lenses in front of your
eyes and measures how they focus light. This is performed using a hand
held lighted instrument called a retinoscope or an automated instrument
that automatically evaluates the focusing power of the eye. The power is
then refined by patient’s responses to determine the lenses that allow
the clearest vision.
Using the information obtained from these tests,
your optometrist can determine if you have astigmatism. These findings,
combined with those of other tests performed, will allow the optometrist
to determine the power of any lens correction needed to provide clear,
comfortable vision, and discuss options for treatment.
How is astigmatism treated?
Persons with astigmatism have several options
available to regain clear vision. They include:
eyeglasses
contact lenses
orthokeratology
laser and other refractive surgery procedures
 Eyeglasses are a common form of correction for persons with astigmatism. Eyeglasses are a common form of correction for persons with astigmatism.
Eyeglasses are the primary choice of correction for
persons with astigmatism. They will contain a special cylindrical lens
prescription to compensate for the astigmatism. This provides for
additional lens power in only specific meridians of the lens. An example
of a prescription for astigmatism for one eye would be -1.00 -1.25 X
180. The middle number (-1.25) is the lens power for correction of the
astigmatism. The “X 180” designates the placement (axis) of the lens
power. The first number (-1.00) indicates that this prescription also
includes a correction for nearsightedness in addition to astigmatism.
Generally, a single vision lens is prescribed to
provide clear vision at all distances. However, for patients over about
age 40 who have the condition called
presbyopia, a bifocal or
progressive addition lens may be needed. These provide different lens
powers to see clearly in the distance and to focus effectively for near
vision work.
A wide variety of lens types and frame designs are
now available for patients of all ages. Eyeglasses are no longer just a
medical device that provides needed vision correction. Eyeglass frames
are available in a many shapes, sizes, colors and materials that not
only allow for correction of vision, but also enhance appearance.
For some individuals,
contact lenses can
offer better vision than eyeglasses. They may provide clearer vision and
a wider field of view. However, since contact lenses are worn directly
on the eyes, they require regular
cleaning and care to safeguard eye health.
Soft contact lenses conform to the shape of the
eye, therefore standard soft lenses may not be effective in correcting
astigmatism. However, special toric soft contact lenses are available to
provide a correction for many types of astigmatism. Because rigid gas
permeable contact lenses maintain their regular shape while on the
cornea, they offer an effective way to compensate for the cornea’s
irregular shape and improve vision for persons with astigmatism and
other refractive errors.
Orthokeratology (Ortho-K) involves the fitting of a series of rigid
contact lenses to reshape the cornea, the front outer cover of the eye.
The contact lenses are worn for limited periods, such as overnight, and
then removed. Persons with moderate amounts of astigmatism may be able
to temporarily obtain clear vision without lenses for most of their
daily activities. Orthokeratology does not permanently improve vision
and if you stop wearing the retainer lenses, your vision may return to
its original condition.
Astigmatism can also be corrected by
reshaping the cornea using a
highly focused laser beam of light. Two commonly used procedures are
photorefractive keratectomy (PRK) and laser in situ keratomileusis
(LASIK).
PRK removes tissue from the superficial and inner
layers of the cornea. LASIK does not remove tissue from the surface of
the cornea, but only from its inner layer. To do this, a section of
outer corneal surface is cut and folded back to expose the inner tissue.
Then a laser is used to remove the precise amount of tissue needed and
the flap of outer tissue is placed back in position to heal. Both
procedures allow light to focus on the retina by altering the shape of
the cornea.
Individuals with astigmatism have a wide range of
options to correct their vision problem. In consultation with your
optometrist, you can select the treatment that best meets your visual
and lifestyle needs.
|
Blepharitis
|
Blepharitis is an inflammation of the eyelids
causing red, irritated, itchy eyelids and the formation of dandruff-like
scales on eyelashes. It is a common eye disorder caused by either
bacterial or a skin condition such as dandruff of the scalp or acne
rosacea. It affects people of all ages. Although uncomfortable,
blepharitis is not contagious and generally does not cause any permanent
damage to eyesight.
Blepharitis is classified into two types:
Anterior blepharitis occurs at the outside front
edge of the eyelid where the eyelashes are attached.
Posterior blepharitis affects the inner edge of the
eyelid that comes in contact with the eyeball.
Individuals with blepharitis may experience a
gritty or burning sensation in their eyes, excessive tearing, itching,
red and swollen eyelids, dry eyes, or crusting of the eyelids. For some
people, blepharitis causes only minor irritation and itching. However,
it can lead to more severe signs and symptoms such as blurring of
vision, missing or misdirected eyelashes, and inflammation of other eye
tissue, particularly the cornea.
In many cases, good eyelid hygiene and a regular
cleaning routine can control blepharitis. This includes frequent scalp
and face washing, using warm compresses to soak the eyelids, and doing
eyelid scrubs. In cases where a bacterial infection is the cause,
various antibiotics and other medications may be prescribed along with
eyelid hygiene.
What causes blepharitis?
 Blepharitis can appear as greasy flakes or scales around the base of the Blepharitis can appear as greasy flakes or scales around the base of the
eyelashes.
Anterior blepharitis is commonly caused by bacteria
(staphylococcal blepharits) or dandruff of the scalp and eyebrows
(seborrheic blepharitis). It may also occur due to a combination of
factors, or less commonly may be the result of allergies or an
infestation of the eyelashes.
Posterior blepharitis can be caused by irregular
oil production by the glands of the eyelids (meibomian blepharitis)
which creates a favorable environment for bacterial growth. It can also
develop as a result of other skin conditions such as acne rosacea and
scalp dandruff.
How is blepharitis diagnosed?
Blepharitis can be diagnosed through a
comprehensive eye examination.
Testing, with special emphasis on evaluation of the eyelids and front
surface of the eyeball, may include:
Patient history to determine any symptoms the
patient is experiencing and the presence of any general health problems
that may be contributing to the eye problem.
External examination of the eye, including lid
structure, skin texture and eyelash appearance.
Evaluation of the lid margins, base of the
eyelashes and meibomian gland openings using bright light and
magnification.
Evaluation of the quantity and quality of tears for
any abnormalities.
A differentiation among the various types of
blepharitis can often be made based on the appearance of the eyelid
margins:
Staphyloccal blepharitis patients frequently
exhibit mild sticking together of the lids, thickened lid margins, and
missing and misdirected eyelashes.
Seborrheic blepharitis appears as greasy flakes or
scales around the base of eyelashes and a mild redness of the eyelids.
Ulcerative blepharitis is characterized by matted,
hard crusts around the eyelashes that when removed, leave small sores
that ooze and bleed. There may also be a loss of eyelashes, distortion
of the front edges of the eyelids and chronic tearing. In severe cases,
the cornea, the transparent front covering of the eyeball, may also
become inflamed.
Meibomian blepharitis is evident by blockage of the
oil glands in the eyelids, poor quality of tears, and redness of the
lining of the eyelids.
Using the information obtained from testing, your
optometrist can determine if you have blepharitis and advise you on
treatment options.
How is blepharitis treated?
Treatment depends on the specific type of
blepharitis. The key to treating most types of blepharitis is keeping
the lids clean and free of crusts.

Limiting or stopping the use of eye makeup when treating blepharitis is
often recommended, as its use will make lid hygiene more difficult.
Warm compresses can be applied to loosen the
crusts, followed by gentle scrubbing of the eyes with a mixture of water
and baby shampoo or an over-the-counter lid cleansing product. In cases
involving bacterial infection, an antibiotic may also be prescribed.
If the glands in the eyelids are blocked, the
eyelids may need to be massaged to clean out oil accumulated in the
eyelid glands.
Artificial tear solutions or lubricating ointments
may be prescribed in some cases.
Use of an anti-dandruff shampoo on the scalp can
help.
Limiting or stopping the use of eye makeup is often
recommended, as its use will make lid hygiene more difficult.
If you wear contact lenses, you may have to
temporarily discontinue wearing them during treatment.
Some cases of blepharitis may require more complex
treatment plans. Blepharitis seldom disappears completely. Even with
successful treatment, relapses may occur.
Blepharitis seldom disappears completely. Even with
successful treatment, relapses may occur.
Self-care
An important part of controlling blepharitis
involves treatment at home.
Directions for a Warm Soak of the Eyelids:
Wash your hands thoroughly.
Moisten a clean washcloth with warm water.
Close eyes and place washcloth on eyelids for about
5 minutes, reheating the washcloth as necessary.
Repeat several times daily.
Directions for an Eyelid Scrub:
Wash your hands thoroughly.
Mix warm water and a small amount of non-irritating
(baby) shampoo or use a commercially prepared lid scrub solution
recommended by your optometrist.
Using a clean cloth (a different one for each eye)
rub the solution back and forth across the eyelashes and edge of the
closed eyelid.
Rinse with clear water.
Repeat with the other eye.
|
Cataract
|
A cataract is a cloudy or opaque area in the
normally clear lens of the eye. Depending upon its size and location, it
can interfere with normal vision. Most cataracts develop in people over
age 55, but they occasionally occur in infants and young children.
Usually cataracts develop in both eyes, but one may be worse than the
other. Reasearchers have linked eye-friendly nutrients such as
lutein/zeaxanthin,
vitamin C,
vitamin E, and
zinc to reducing the risk of
certain eye diseases, including cataracts. For more information on the
importance of good nutrition and eye health, please see the
diet and nutrition section.
The lens is located inside the eye behind the iris,
the colored part of the eye. The lens focuses light on the back of the
eye, the retina. The lens is made of mostly proteins and water. Clouding
of the lens occurs due to changes in the proteins and lens fibers.
The lens is composed of layers like an onion. The
outermost is the capsule. The layer inside the capsule is the cortex,
and the innermost layer is the nucleus. A cataract may develop in any of
these areas and is described based on its location in the lens:
A nuclear cataract is located in the center of the
lens. The nucleus tends to darken changing from clear to yellow and
sometimes brown.
A cortical cataract affects the layer of the lens
surrounding the nucleus. It is identified by its unique wedge or spoke
appearance.
A posterior capsular cataract is found in the back
outer layer of the lens. This type often develops more rapidly.
|
Types of Cataracts
|
|

|

|

|
|
Nuclear cataract
|
Cortical cataract
|
Posterior capsular cataract
|
Normally, the lens focuses light on the retina,
which sends the image through the optic nerve to the brain. However, if
the lens is clouded by a cataract, light is scattered so the lens can no
longer focus it properly, causing vision problems.
Cataracts generally form very slowly. Signs and
symptoms of a cataract may include:
Blurred or hazy vision
Reduced intensity of colors
Increased sensitivity to glare from lights,
particularly when driving at night
Increased difficulty seeing at night
Change in the eye’s refractive error
While the process of cataract formation is becoming
more clearly understood, there is no clinically established treatment to
prevent or slow their progression. In age-related cataracts, changes in
vision can be very gradual. Some people may not initially recognize the
visual changes. However, as cataracts worsen vision symptoms tend to
increase in severity.
|
Chalazion
|
A chalazion is a slowly developing lump that forms
due to blockage and swelling of an oil gland in the eyelid. It is more
common in adults than children and occurs most frequently in persons 30
to 50 years of age.
Initially, a chalazion may appear as a red, tender,
swollen area of the eyelid. However, in a few days it changes to a
painless, slow growing lump in the eyelid. A chalazion often starts out
very small and is barely able to be seen, but it may grow to the size of
a pea. Often times they may be confused with sties, which are also areas
of swelling in the eyelid.
A sty is an infection of an oil gland in the
eyelid. It produces a red, swollen, painful lump on the edge or inside
surface of the eyelid. Sties usually occur closer to the surface of the
eyelid than do chalazia.
A chalazion is generally not due to an infection,
but results from a blockage of the oil gland itself. However, a
chalazion may occur as an after-effect of a sty.
Common signs or symptoms of a chalazion include:
Appearance of a painless bump or lump in the upper
eyelid, or, less commonly, in the lower eyelid
Tearing
Blurred vision, if the chalazion is large enough to
press against the eyeball
Most chalazia disappear without treatment in
several weeks to a month. However, they often recur. Rarely, they may be
an indication of an infection or skin cancer.
What causes a chalazion?
A chalazion can develop when the oil produced by
glands within the eyelids, called the meibomian glands, becomes
thickened and is unable to flow out of the gland. The oil builds up
inside the gland and forms a lump in the eyelid. Eventually the gland
may break open and release the oil into the surrounding tissue causing
an inflammation of the eyelid.
Risk factors for the development of a chalazion
include:
Chronic blepharitis, an inflammation of the eyelids
and eye lashes
Acne rosacea
Seborrhea
Tuberculosis
Viral infection
How is a chalazion diagnosed?
A chalazion can be diagnosed through a
comprehensive eye examination. Testing, with special emphasis on
evaluation of the eyelids, may include:
Patient history to determine any symptoms the
patient is experiencing and the presence of any general health problems
that may be contributing to the eye problem.
External examination of the eye, including lid
structure, skin texture and eyelash appearance.
Evaluation of the lid margins, base of the
eyelashes and oil gland openings using bright light and magnification.
Using the information obtained from testing, your
optometrist can determine if you have a chalazion and advise you on
treatment options.
How is a chalazion treated?
Many chalazia require minimal medical treatment,
resolving on their own in a few weeks to a month. To facilitate healing,
warm compresses can be applied to the eyelid for 10 to15 minutes 4 to 6
times a day for several days. The warm compresses may help soften the
hardened oil that is blocking the ducts thereby promoting drainage and
healing. Lightly messaging the external area of the eyelid for several
minutes each day may also help to promote drainage.
A clean soft cloth dipped in warm water and wrung
out can serve as an effective compress. Remoisten the cloth frequently
to keep it wet and warm. Once the chalazion drains on its own, keep the
area clean and keep your hands away from your eyes.
If the chalazion does not drain and heal within a
month, contact your eye doctor. Don’t attempt to squeeze or drain the
chalazion yourself.
|
Color Vision Deficiency
|
Color vision deficiency is the inability to
distinguish certain shades of color or in more severe cases, see colors
at all. The term “color blindness” is also used to describe this visual
condition, but very few people are completely color blind.
 Red-green deficiency results in the inability to distinguish certain Red-green deficiency results in the inability to distinguish certain
shades of red and green. Most people with color vision deficiency can see
colors, but they have difficulty differentiating between
particular shades of reds and greens (most common)
or
blues and yellows (less common).
People who are totally color blind, a condition
called achromatopsia, can only see things as black and white or in
shades of gray.
The severity of color vision deficiency can range
from mild to severe depending on the cause. It will affect both eyes if
it is inherited and usually just one if the cause for the deficiency is
injury or illness.
Color vision is possible due to photoreceptors in
the retina of the eye known as cones. These cones have light sensitive
pigments that enable us to recognize color. Found in the macula, the
central portion of the retina, each cone is sensitive to either red,
green or blue light, which the cones recognize based upon light
wavelengths.
Normally, the pigments inside the cones register
differing colors and send that information through the optic nerve to
the brain enabling you to distinguish countless shades of color. But if
the cones lack one or more light sensitive pigments, you will be unable
to see one or more of the three primary colors thereby causing a
deficiency in your color perception.
The most common form of color deficiency is
red-green. This does not mean that people with this deficiency cannot
see these colors at all; they simply have a harder time differentiating
between them. The difficulty they have in correctly identifying them
depends on how dark or light the colors are.
Another form of color deficiency is blue-yellow.
This is a rarer and more severe form of color vision loss than red-green
since persons with blue-yellow deficiency frequently have red-green
blindness too. In both cases, it is common for people with color vision
deficiency to see neutral or gray areas where a particular color should
appear.
|
Computer Vision Syndrome
|
A group of eye and vision-related problems that
result from prolonged computer use.
|
Conjunctivitis
|
Conjunctivitis is an inflammation or infection of
the conjunctiva, the thin transparent layer of tissue that lines the
inner surface of the eyelid and covers the white part of the eye.
Conjunctivitis, often called “pink eye,” is a common eye disease,
especially in children. It may affect one or both eyes. Some forms of
conjunctivitis can be highly contagious and easily spread in schools and
at home. While conjunctivitis is usually a minor eye infection,
sometimes it can develop into a more serious problem.
Conjunctivitis may be caused by a viral or
bacterial infection. It can also occur due to an allergic reaction to
irritants in the air like pollen and smoke, chlorine in swimming pools,
and ingredients in cosmetics or other products that come in contact with
the eyes. Sexually transmitted diseases like Chlamydia and gonorrhea are
less common causes of conjunctivitis.
People with conjunctivitis may experience the
following symptoms:
A gritty feeling in one or both eyes
Itching or burning sensation in one or both eyes
Excessive tearing
Discharge coming from one or both eyes
Swollen eyelids
Pink discoloration to the whites of one or both
eyes
Increased sensitivity to light
What causes conjunctivitis?

Allergic Conjunctivitis occurs more commonly among people who already
have seasonal allergies.
The cause of conjunctivitis varies depending on the
offending agent. There are three main categories of conjunctivitis:
allergic, infectious and chemical:
Allergic Conjunctivitis
Allergic Conjunctivitis occurs more commonly among
people who already have seasonal allergies. At some point they come into
contact with a substance that triggers an allergic reaction in their
eyes.
Giant Papillary Conjunctivitis is a type of
allergic conjunctivitis caused by the chronic presence of a foreign body
in the eye. This condition occurs predominantly with people who wear
hard or rigid contact lenses, wear soft contact lenses that are not
replaced frequently, have an exposed suture on the surface or the eye,
or have a glass eye.
Infectious Conjunctivitis
Bacterial Conjunctivitis is an infection most often
caused by staphylococcal or streptococcal bacteria from your own skin or
respiratory system. Infection can also occur by transmittal from
insects, physical contact with other people, poor hygiene (touching the
eye with unclean hands), or by use of contaminated eye makeup and facial
lotions.
Viral Conjunctivitis is most commonly caused by
contagious viruses associated with the common cold. The primary means of
contracting this is through exposure to coughing or sneezing by persons
with upper respiratory tract infections. It can also occur as the virus
spreads along the body’s own mucous membranes connecting lungs, throat,
nose, tear ducts, and conjunctiva.
Ophthalmia Neonatorum is a severe form of bacterial
conjunctivitis that occurs in newborn babies. This is a serious
condition that could lead to permanent eye damage unless it is treated
immediately. Ophthalmia neonatorum occurs when an infant is exposed to
Chlamydia or gonorrhea while passing through the birth canal.
Chemical Conjunctivitis
Chemical Conjunctivitis can be caused by irritants
like air pollution, chlorine in swimming pools, and exposure to noxious
chemicals.
How is conjunctivitis diagnosed?

Conjunctivitis can be diagnosed through a comprehensive eye examination.
Conjunctivitis can be diagnosed through a
comprehensive eye examination. Testing, with special emphasis on
evaluation of the conjunctiva and surrounding tissues, may include:
Patient history to determine the symptoms the
patient is experiencing, when the symptoms began, and the presence of
any general health or environmental conditions that may be contributing
to the problem.
Visual acuity measurements to determine the extent
to which vision may be affected.
Evaluation of the conjunctiva and external eye
tissue using bright light and magnification.
Evaluation of the inner structures of the eye to
ensure that no other tissues are affected by the condition.
Supplemental testing may include taking cultures or
smears of conjunctival tissue, particularly in cases of chronic
conjunctivitis or when the condition is not responding to treatment.
Using the information obtained from these tests,
your optometrist can determine if you have conjunctivitis and advise you
on treatment options.
How is conjunctivitis treated?
Treatment of conjunctivitis is directed at three
main goals:
To increase patient comfort.
To reduce or lessen the course of the infection or
inflammation.
To prevent the spread of the infection in
contagious forms of conjunctivitis.
The appropriate treatment for conjunctivitis
depends on its cause:
Allergic conjunctivitis – The first step should be
to remove or avoid the irritant, if possible. Cool compresses and
artificial tears sometimes relieve discomfort in mild cases. In more
severe cases, non-steroidal anti-inflammatory medications and
antihistamines may be prescribed. Cases of persistent allergic
conjunctivitis may also require topical steroid eye drops.
Bacterial conjunctivitis – This type of
conjunctivitis is usually treated with antibiotic eye drops or
ointments. Improvement can occur after three or four days of treatment,
but the entire course of antibiotics needs to be used to prevent
recurrence.
Viral Conjunctivitis – There are no available drops
or ointments to eradicate the virus for this type of conjunctivitis.
Antibiotics will not cure a viral infection. Like a common cold, the
virus just has to run its course, which may take up to two or three
weeks in some cases. The symptoms can often be relieved with cool
compresses and artificial tear solutions. For the worst cases, topical
steroid drops may be prescribed to reduce the discomfort from
inflammation, but do not shorten the course of the infection. Some
doctors may perform an ophthalmic iodine eye wash in the office in hopes
of shortening the course of the infection. This newer treatment has not
been well studied yet, therefore no conclusive evidence of the success
exists.
Chemical Conjunctivitis – Treatment for chemical
conjunctivitis requires careful flushing of the eyes with saline and may
require topical steroids. The more acute chemical injuries are medical
emergencies, particularly alkali burns, which can lead to severe
scarring, intraocular damage or even loss of the eye.
Contact Lens Wearers

Contact lens wearers may need to discontinue wearing their lenses while
the conjunctivitis is active.
Contact lens wearers may need to discontinue
wearing their lenses while the condition is active. Your doctor can
advise you on the need for temporary restrictions on contact lens wear.
If the conjunctivitis developed due to wearing
contact lenses, your eye doctor may recommend that you switch to a
different type of contact lens or disinfection solution. Your
optometrist might need to alter your contact lense prescription to a
type of lens that you replace more frequently to prevent the
conjunctivitis from recurring.
Self-care
Practicing good hygiene is the best way to control
the spread of conjunctivitis. Once an infection has been diagnosed,
follow these steps:
Don’t touch your eyes with your hands.
Wash your hands thoroughly and frequently.
Change your towel and washcloth daily, and don’t
share them with others.
Discard eye cosmetics, particularly mascara.
Don’t use anyone else’s eye cosmetics or personal
eye-care items.
Follow your eye doctor’s instructions on proper
contact lens care.
You can soothe the discomfort of viral or bacterial
conjunctivitis by applying warm compresses to your affected eye or eyes.
To make a compress, soak a clean cloth in warm water and wring it out
before applying it gently to your closed eyelids.
For allergic conjunctivitis, avoid rubbing your
eyes. Instead of warm compresses, use cool compresses to soothe your
eyes. Over the counter eye drops are available. Antihistamine eye drops
should help to alleviate the symptoms, and lubricating eye drops help to
rinse the allergen off of the surface of the eye.
See your doctor of optometry when you experience
conjunctivitis to help diagnose the cause and the proper course of
action.
|
Convergence Insufficiency
|
An eye coordination problem in which the eyes have
a tendency to drift outward when reading or doing close work.
|
Corneal Abrasion
|
A cut or scratch on the cornea, the clear front
cover of the eye.
|
Crossed Eyes
|
A condition in which both eyes do not look at the
same place at the same time. See also Amblyopia.
|
Diabetic Retinopathy
|
Diabetic retinopathy is a condition occurring in
persons with diabetes, which causes progressive damage to the retina,
the light sensitive lining at the back of the eye. It is a serious
sight-threatening complication of diabetes.
Diabetes is a disease that interferes with the
body’s ability to use and store sugar, which can cause many health
problems. Too much sugar in the blood can cause damage throughout the
body, including the eyes. Over time, diabetes affects the circulatory
system of the retina.
Diabetic retinopathy is the result of damage to the
tiny blood vessels that nourish the retina. They leak blood and other
fluids that cause swelling of retinal tissue and clouding of vision. The
condition usually affects both eyes. The longer a person has diabetes,
the more likely they will develop diabetic retinopathy. If left
untreated, diabetic retinopathy can cause blindness.
Symptoms of diabetic retinopathy include:
Seeing spots or floaters in your field of vision
Blurred vision
Having a dark or empty spot in the center of your
vision
Difficulty seeing well at night
In patients with diabetes, prolonged periods of
high blood sugar can lead to the accumulation of fluid in the lens
inside the eye that controls eye focusing. This changes the curvature of
the lens and results in the development of symptoms of blurred vision.
The blurring of distance vision as a result of lens swelling will
subside once the blood sugar levels are brought under control. Better
control of blood sugar levels in patients with diabetes also slows the
onset and progression of diabetic retinopathy.
Often there are no visual symptoms in the early
stages of diabetic retinopathy. That is why the American Optometric
Association recommends that everyone with diabetes have a comprehensive
dilated eye examination once a year. Early detection and treatment can
limit the potential for significant vision loss from diabetic
retinopathy.
Treatment of diabetic retinopathy varies depending
on the extent of the disease. It may require laser surgery to seal
leaking blood vessels or to discourage new leaky blood vessels from
forming. Injections of medications into the eye may be needed to
decrease inflammation or stop the formation of new blood vessels. In
more advanced cases, a surgical procedure to remove and replace the
gel-like fluid in the back of the eye, called the vitreous, may be
needed. A retinal detachment, defined as a separation of the
light-receiving lining in the back of the eye, resulting from diabetic
retinopathy, may also require surgical repair.
If you are a diabetic, you can help prevent or slow
the development of diabetic retinopathy by taking your prescribed
medication, sticking to your diet, exercising regularly, controlling
high blood pressure and avoiding alcohol and smoking.
What causes diabetic retinopathy?

Non-proliferative diabetic retinopathy (NPDR) is the early state of the
disease in which symptoms will be mild or non-existent. In NPDR, the
blood vessels in the retina are weakened causing tiny bulges called
microanuerysms to protrude from their walls.
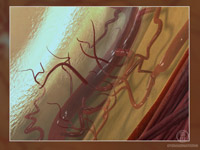
Proliferative diabetic retinopathy (PDR) is the more advanced form of
the disease. At this stage, new fragile blood vessels can begin to grow
in the retina and into the vitreous, the gel-like fluid that fills the
back of the eye. The new blood vessel may leak blood into the vitreous,
clouding vision.
Diabetic retinopathy is the result of damage caused by diabetes to the
small blood vessels located in the retina. Blood vessels damaged from
diabetic retinopathy can cause vision loss:
Fluid can leak into the macula, the area of the
retina which is responsible for clear central vision. Although small,
the macula is the part of the retina that allows us to see colors and
fine detail. The fluid causes the macula to swell, resulting in blurred
vision.
In an attempt to improve blood circulation in the
retina, new blood vessels may form on its surface. These fragile,
abnormal blood vessels can leak blood into the back of the eye and block
vision.
Diabetic retinopathy is classified into two types:
Non-proliferative diabetic retinopathy (NPDR) is
the early state of the disease in which symptoms will be mild or
non-existent. In NPDR, the blood vessels in the retina are weakened
causing tiny bulges called microanuerysms to protrude from their walls.
The microanuerysms may leak fluid into the retina, which may lead to
swelling of the macula.
Proliferative diabetic retinopathy (PDR) is the
more advanced form of the disease. At this stage, circulation problems
cause the retina to become oxygen deprived. As a result new fragile
blood vessels can begin to grow in the retina and into the vitreous, the
gel-like fluid that fills the back of the eye. The new blood vessel may
leak blood into the vitreous, clouding vision. Other complications of
PDR include detachment of the retina due to scar tissue formation and
the development of glaucoma. Glaucoma is an eye disease defined as
progressive damage to the optic nerve. In cases of proliferative
diabetic retinopathy, the cause of this nerve damage is due to extremely
high pressure in the eye. If left untreated, proliferative diabetic
retinopathy can cause severe vision loss and even blindness.
Risk factors for diabetic retinopathy include:
Diabetes — people with Type 1 or Type 2 diabetes
are at risk for the development of diabetic retinopathy. The longer a
person has diabetes, the more likely they are to develop diabetic
retinopathy, particularly if the diabetes is poorly controlled.
Race — Hispanic and African Americans are at
greater risk for developing diabetic retinopathy.
Medical conditions — persons with other medical
conditions such as high blood pressure and high cholesterol are at
greater risk.
Pregnancy — pregnant women face a higher risk for
developing diabetes and diabetic retinopathy. If gestational diabetes
develops, the patient is at much higher risk of developing diabetes as
they age.
How is diabetic retinopathy diagnosed?

Diabetic retinopathy can be diagnosed through a comprehensive eye
examination.
Diabetic retinopathy can be diagnosed through a
comprehensive eye examination.
Testing, with special emphasis on evaluation of the retina and macula,
may include:
Patient history to determine vision difficulties
experienced by the patient, presence of diabetes, and other general
health concerns that may be affecting vision
Visual acuity measurements to determine the extent
to which central vision has been affected
Refraction to determine the need for changes in an
eyeglass prescription
Evaluation of the ocular structures, including the
evaluation of the retina through a dilated pupil
Measurement of the pressure within the eye
Supplemental testing may include:
Retinal photography or tomography to document
current status of the retina
Fluorescein angiography to evaluate abnormal blood
vessel growth
How is diabetic retinopathy treated?
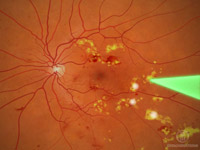
Laser treatment (photocoagulation) is used to stop the leakage of blood
and fluid into the retina. A laser beam of light can be used to create
small burns in areas of the retina with abnormal blood vessels to try to
seal the leaks.
Treatment for diabetic retinopathy depends on the stage of the disease
and is directed at trying to slow or stop the progression of the
disease.
In the early stages of Non-proliferative Diabetic
Retinopathy, treatment other than regular monitoring may not be
required. Following your doctor’s advice for diet and exercise and
keeping blood sugar levels well-controlled can help control the
progression of the disease.
If the disease advances, leakage of fluid from
blood vessels can lead to macular edema. Laser treatment
(photocoagulation) is used to stop the leakage of blood and fluid into
the retina. A laser beam of light can be used to create small burns in
areas of the retina with abnormal blood vessels to try to seal the
leaks.
When blood vessel growth is more widespread
throughout the retina, as in proliferative diabetic retinopathy, a
pattern of scattered laser burns is created across the retina. This
causes abnormal blood vessels to shrink and disappear. With this
procedure, some side vision may be lost in order to safeguard central
vision.
Some bleeding into the vitreous gel may clear up on
its own. However, if significant amounts of blood leak into the vitreous
fluid in the eye, it will cloud vision and can prevent laser
photocoagulation from being used. A surgical procedure called a
vitrectomy may be used to remove the blood-filled vitreous and replace
it with a clearfluid to maintain the normal shape and health of the eye.
Persons with diabetic retinopathy can suffer
significant vision loss. Special low vision devices such as telescopic
and microscopic lenses, hand and stand magnifiers, and video
magnification systems can be prescribed to make the most of remaining
vision.
|
Dry Eye
|
Dry eye is a condition in which there are
insufficient tears to lubricate and nourish the eye. Tears are necessary
for maintaining the health of the front surface of the eye and for
providing clear vision. People with dry eyes either do not produce
enough tears or have a poor quality of tears. Dry eye is a common and
often chronic problem, particularly in older adults.
With each blink of the eyelids, tears are spread
across the front surface of the eye, known as the cornea. Tears provide
lubrication, reduce the risk of eye infection, wash away foreign matter
in the eye, and keep the surface of the eyes smooth and clear. Excess
tears in the eyes flow into small drainage ducts, in the inner corners
of the eyelids, which drain in the back of the nose.
Dry eyes can result from an improper balance of
tear production and drainage.
Inadequate amount of tears – Tears are produced by
several glands in and around the eyelids. Tear production tends to
diminish with age, with various medical conditions, or as a side effect
of certain medicines. Environmental conditions such as wind and dry
climates can also affect tear volume by increasing tear evaporation.
When the normal amount of tear production decreases or tears evaporate
too quickly from the eyes, symptoms of dry eye can develop.
 Poor Poor
quality of tears – Tears are made up of three layers: oil, water, and
mucus. Each component serves a function in protecting and nourishing the
front surface of the eye. A smooth oil layer helps to prevent
evaporation of the water layer, while the mucin layer functions in
spreading the tears evenly over the surface of the eye. If the tears
evaporate too quickly or do not spread evenly over the cornea due to
deficiencies with any of the three tear layers, dry eye symptoms can
develop.
The most common form of dry eyes is due to an
inadequate amount of the water layer of tears. This condition, called
keratoconjunctivitis sicca (KCS), is also referred to as dry eye
syndrome.
People with dry eyes may experience symptoms of
irritated, gritty, scratchy, or burning eyes, a feeling of something in
their eyes, excess watering, and blurred vision. Advanced dry eyes may
damage the front surface of the eye and impair vision.
Treatments for dry eyes aim to restore or maintain
the normal amount of tears in the eye to minimize dryness and related
discomfort and to maintain eye health.
What causes dry eyes?

The majority of people over the age of 65 experience some symptoms of
dry eyes.
The development of dry eyes can have many causes.
They include:
Age – dry eye is a part of the natural aging
process. The majority of people over age 65 experience some symptoms of
dry eyes.
Gender – women are more likely to develop dry eyes
due to hormonal changes caused by pregnancy, the use of oral
contraceptives, and menopause.
Medications – certain medicines, including
antihistamines, decongestants, blood pressure medications and
antidepressants, can reduce the amount of tears produced in the eyes.
Medical conditions – persons with rheumatoid
arthritis, diabetes and thyroid problems are more likely to have
symptoms of dry eyes. Also, problems with inflammation of the eyelids (blepharitis),
inflammation of the surfaces of the eye, or the inward or outward
turning of eyelids can cause dry eyes to develop.
Environmental conditions – exposure to smoke, wind
and dry climates can increase tear evaporation resulting in dry eye
symptoms. Failure to blink regularly, such as when staring at a computer
screen for long periods of time, can also contribute to drying of the
eyes.
Other factors – long term use of contact lenses can
be a factor in the development of dry eyes. Refractive eye surgeries,
such as LASIK, can cause decreased tear production and dry eyes.
How are dry eyes diagnosed?
Dry eyes can be diagnosed through a comprehensive
eye examination. Testing, with special emphasis on the evaluation of the
quantity and quality of tears produced by the eyes, may include:
Patient history to determine any symptoms the
patient is experiencing and the presence of any general health problems,
medications taken, or environmental factors that may be contributing to
the dry eye problem.
External examination of the eye, including lid
structure and blink dynamics.
Evaluation of the eyelids and cornea using bright
light and magnification.
Measurement of the quantity and quality of tears
for any abnormalities. Special dyes may be instilled in the eyes to
better observe tear flow and to highlight any changes to the outer
surface of the eye caused by insufficient tears.
Using the information obtained from testing, your
optometrist can determine if you have dry eyes and advise you on
treatment options.
How are dry eyes treated?

One of the primary approaches used to manage and treat mild cases of dry
eyes is adding tears using over-the-counter artificial tear solutions.
Dry eyes can be a chronic condition, but your
optometrist can prescribe treatment to keep your eyes healthy, more
comfortable, and prevent your vision from being affected. The primary
approaches used to manage and treat dry eyes include adding tears,
conserving tears, increasing tear production, and treating the
inflammation of the eyelids or eye surface that contributes to the dry
eyes.
Adding tears – Mild cases of dry eyes can often be
managed using over-the-counter artificial tear solutions. These can be
used as often as needed to supplement natural tear production.
Preservative-free artificial tear solutions are recommended because they
contain fewer additives that could further irritate the eyes. However,
some people may have persistent dry eyes that don’t respond to
artificial tears alone. Additional steps need to be taken to treat their
dry eyes.
Conserving tears – An additional approach to
reducing the symptoms of dry eyes is to keep natural tears in the eyes
longer. This can be done by blocking the tear ducts through which the
tears normally drain. The tear ducts can be blocked with tiny silicone
or gel-like plugs that can be removed, if needed. A surgical procedure
to permanently close tear ducts can also be used. In either case, the
goal is to keep the available tears in the eye longer to reduce problems
related to dry eyes.
Increasing tear production – Prescription eye drops
that help to increase production of tears can be recommended by your
optometrist, as well as omega-3 fatty acid nutritional supplements.
Treatment of the contributing eyelid or ocular
surface inflammation – Prescription eye drops or ointments, warm
compresses and lid massage, or eyelid cleaners may be recommended to
help decrease inflammation around the surface of the eyes.
Self Care
Steps you can take to reduce symptoms of dry eyes
include:
Remembering to blink regularly when reading or
staring at a computer screen for long periods of time.
Increasing the level of humidity in the air at work
and at home.
Wearing sunglasses outdoors, particularly those
with wrap around frame design, to reduce exposure to drying winds and
sun.
Using nutritional supplements containing essential
fatty acids may help decrease dry eye symptoms in some people. Ask your
optometrist if the use of dietary supplements could be of help for your
dry eye problems.
Avoiding becoming dehydrated by drinking plenty of
water (8 to 10 glasses) each day.
|
Farsightedness (Hyperopia)
|
Farsightedness, or hyperopia, as it is medically
termed, is a vision condition in which distant objects are usually seen
clearly, but close ones do not come into proper focus. Farsightedness
occurs if your eyeball is too short or the cornea has too little
curvature, so light entering your eye is not focused correctly.
Common signs of farsightedness include difficulty
in concentrating and maintaining a clear focus on near objects, eye
strain, fatigue and/or headaches after close work, aching or burning
eyes, irritability or nervousness after sustained concentration.
Common vision screenings, often done in schools,
are generally ineffective in detecting farsightedness. A comprehensive
optometric examination will include testing for farsightedness.
In mild cases of farsightedness, your eyes may be
able to compensate without corrective lenses. In other cases, your
optometrist can prescribe eyeglasses or contact lenses to optically
correct farsightedness by altering the way the light enters your eyes.
|
Floaters & Spots
|
Spots (often called floaters) are small,
semi-transparent or cloudy specks or particles within the vitreous,
which is the clear, jelly-like fluid that fills the inside of your eyes.
They appear as specks of various shapes and sizes, threadlike strands or
cobwebs. Because they are within your eyes, they move as your eyes move
and seem to dart away when you try to look at them directly.
Spots are often caused by small flecks of protein
or other matter trapped during the formation of your eyes before birth.
They can also result from deterioration of the vitreous fluid, due to
aging; or from certain eye diseases or injuries.
Most spots are not harmful and rarely limit vision.
But, spots can be indications of more serious problems, and you should
see your optometrist for a comprehensive examination when you notice
sudden changes or see increases in them.
By looking in your eyes with special instruments,
your optometrist can examine the health of your eyes and determine if
what you are seeing is harmless or the symptom of a more serious problem
that requires treatment.

Most spots are not harmful and rarely limit vision. But, spots can be
indications of more serious problems.
|
Glaucoma
|
Glaucoma is a group of eye disorders leading to
progressive damage to the optic nerve, and is characterized by loss of
nerve tissue resulting in loss of vision. The optic nerve is a bundle of
about one million individual nerve fibers and transmits the visual
signals from the eye to the brain. The most common form of glaucoma,
primary open-angle glaucoma, is associated with an increase in the fluid
pressure inside the eye. This increase in pressure may cause progressive
damage to the optic nerve and loss of nerve fibers. Vision loss may
result. Advanced glaucoma may even cause blindness. Not everyone with
high eye pressure will develop glaucoma, and many people with normal eye
pressure will develop glaucoma. When the pressure inside an eye is too
high for that particular optic nerve, whatever that pressure measurement
may be, glaucoma will develop.
Glaucoma is the second leading cause of blindness in the U.S. It most
often occurs in people over age 40, although a congenital or infantile
form of glaucoma exists. People with a family history of glaucoma,
African Americans over the age of 40, and Hispanics over the age of 60
are at an increased risk of developing glaucoma. Other risk factors
include thinner corneas, chronic eye inflammation, and using medications
that increase the pressure in the eyes.
The most common form of glaucoma, primary
open-angle glaucoma, develops slowly and usually without any symptoms.
Many people do not become aware they have the condition until
significant vision loss has occurred. It initially affects peripheral or
side vision, but can advance to central vision loss. If left untreated,
glaucoma can lead to significant loss of vision in both eyes, and may
even lead to blindness.
A less common type of glaucoma, acute angle closure
glaucoma, usually occurs abruptly due to a rapid increase of pressure in
the eye. Its symptoms may include severe eye pain, nausea, redness in
the eye, seeing colored rings around lights, and blurred vision. This
condition is an ocular emergency, and medical attention should be sought
immediately, as severe vision loss can occur quickly.
Glaucoma cannot currently be prevented, but if
diagnosed and treated early it can usually be controlled. Medication or
surgery can slow or prevent further vision loss. However, vision already
lost to glaucoma cannot be restored. That is why the American Optometric
Association recommends an annual dilated eye examination for people at
risk for glaucoma as a preventive eye care measure. Depending on your
specific condition, your doctor may recommend more frequent
examinations.
What causes glaucoma?

Glaucoma is the leading cause of blindness among Hispanics.
There are many types of glaucoma and many theories
about the causes of glaucoma. The exact cause is unknown. Although the
disease is usually associated with an increase in the fluid pressure
inside the eye, other theories include lack of adequate blood supply to
the nerve.
Primary open-angle glaucoma – This is the most
common form of glaucoma. One theory is that glaucoma is thought to
develop when the eye’s drainage system becomes inefficient over time.
This leads to an increased amount of fluid and a gradual buildup of
pressure within the eye. Other theories of the cause of the optic nerve
damage include poor perfusion, or blood flow, to the optic nerve. Damage
to the optic nerve is slow and painless and a large portion of vision
can be lost before vision problems are noticed. Other theories also
exist.
Angle-closure glaucoma – This type of glaucoma,
also called closed-angle glaucoma or narrow angle glaucoma, is a less
common form of the disease. It is a medical emergency that can cause
vision loss within a day of its onset.
It occurs when the drainage angle in the eye
(formed by the cornea and the iris) closes or becomes blocked. Many
people who develop this type of glaucoma have a very narrow drainage
angle. With age, the lens in the eye becomes larger, pushing the iris
forward and narrowing the space between the iris and the cornea. As this
angle narrows, the aqueous fluid is blocked from exiting through the
drainage system, resulting in a buildup of fluid and an increase in eye
pressure.
Angle-closure glaucoma can be chronic (progressing
gradually) or acute (appearing suddenly). The acute form occurs when the
iris completely blocks the drainage of the aqueous fluid. In people with
a narrow drainage angle, if their pupils become dilated, the angle may
close and cause a sudden increase in eye pressure. Although an acute
attack often affects only one eye, the other eye may be at risk of an
attack as well.
Secondary glaucoma – This type of glaucoma occurs
as a result of an injury or other eye disease. It may be caused by a
variety of medical conditions, medications, physical injuries, and eye
abnormalities. Infrequently, eye surgery can be associated with
secondary glaucoma.
Normal-tension glaucoma – In this form of glaucoma,
eye pressure remains within what is considered to be the “normal” range,
but the optic nerve is damaged nevertheless. Why this happens is
unknown.
It is possible that people with low-tension
glaucoma may have an abnormally sensitive optic nerve or a reduced blood
supply to the optic nerve caused by a condition such as atherosclerosis,
a hardening of the arteries. Under these circumstances even normal
pressure on the optic nerve may be enough to cause damage.
Risk factors
Certain factors can increase the risk for
developing glaucoma. They include:
Age – People over age 60 are at increased risk for
the disease. For African Americans, however, the increase in risk begins
after age 40. The risk of developing glaucoma increases slightly with
each year of age.
Race – African Americans are significantly more
likely to get glaucoma than are Caucasians, and they are much more
likely to suffer permanent vision loss as a result. People of Asian
descent are at higher risk of angle-closure glaucoma and those of
Japanese descent are more prone to low-tension glaucoma.
Family history of glaucoma – Having a family
history of glaucoma increases the risk of developing glaucoma.
Medical conditions – Some studies indicate that
diabetes may increases the risk of developing glaucoma, as do high blood
pressure and heart disease.
Physical injuries to the eye – Severe trauma, such
as being hit in the eye, can result in immediate increased eye pressure
and future increases in pressure due to internal damage. Injury can also
dislocate the lens, closing the drainage angle, and increasing pressure.
Other eye-related risk factors – Eye anatomy,
namely corneal thickness and optic nerve appearance indicate risk for
development of glaucoma. Conditions such as retinal detachment, eye
tumors, and eye inflammations may also induce glaucoma. Some studies
suggest that high amounts of nearsightedness may also be a risk factor
for the development of glaucoma.
Corticosteroid use – Using corticosteroids for
prolonged periods of time appears to put some people at risk of getting
secondary glaucoma.
How is glaucoma diagnosed?
Glaucoma is diagnosed through a comprehensive eye
examination. To establish a diagnosis of glaucoma, several factors must
be present: Because glaucoma is a progressive disease, meaning it
worsens over time, a change in the appearance of the optic nerve, a loss
of nerve tissue, and a corresponding loss of vision confirm the
diagnosis. Some optic nerves have a suspicious appearance, resembling
nerves with glaucoma, but the patients may have no other risk factors or
signs of glaucoma. These patients should be closely followed with
routine comprehensive exams to monitor for change.
Testing includes:
Patient history to determine any symptoms the
patient is experiencing and the presence of any general health problems
and family history that may be contributing to the problem.
Visual acuity measurements to determine the extent
to which vision may be affected.
Tonometry to measure the pressure inside the eye to
detect increased risk factors for glaucoma.
Pachymetry to measure corneal thickness. People
with thinner corneas are at an increased risk of developing glaucoma.
Visual field testing, also called perimetry, to
check if the field of vision has been affected by glaucoma. This test
measures your side (peripheral) vision and central vision by either
determining the dimmest amount of light that can be detected in various
locations of vision, or by determining sensitivity to targets other than
light, and comparing it to others of similar age.
Evaluation of the retina of the eye, which may
include photographs of the optic nerve, in order to monitor any changes
that might occur over time.
Supplemental testing may include gonioscopy, a
procedure allowing views of the angle anatomy, the area in the eye where
fluid drainage occurs. Serial tonometry may be performed. This is a
procedure acquiring several pressure measurements over time, looking for
changes in the eye pressure throughout the day. Other tests include
using devices to measure nerve fiber thickness, and look for specific
areas of the nerve fiber layer for loss of tissue.
How is glaucoma treated?
The treatment of glaucoma is aimed at reducing
intraocular pressure. The most common first line treatment of glaucoma
is usually prescription eye drops that must be taken regularly. In some
cases, systemic medications, laser treatment, or other surgery may be
required. While there is no cure as yet for glaucoma, early diagnosis
and continuing treatment can preserve eyesight.
Medications – A number of medications are currently
available to treat glaucoma. Typically medications are intended to
reduce elevated intraocular pressure. One may be prescribed a single
medication or a combination of medications. The type of medication may
change if it is not providing enough pressure reduction or if the
patient is experiencing side-effects from the drops.
Surgery involves either laser treatment, making a
drainage flap in the eye, inserting a drainage valve, or destroying the
tissue that creates the fluid in the eye. All procedures aim to reduce
the pressure inside the eye. Surgery may help lower pressure when
medication is not sufficient, however it cannot reverse vision loss.
Laser surgery – Laser trabeculoplasty helps fluid
drain out of the eye. A high-energy laser beam is used to stimulate the
trabecular meshwork to work more efficiently at fluid drainage. The
results may be somewhat temporary, and the procedure may need to be
repeated in the future.
Conventional surgery – If eye drops and laser
surgery aren’t effective in controlling eye pressure, you may need a
filtering procedure called a trabeculectomy. Filtering microsurgery
involves creating a drainage flap, allowing fluid to percolate into and
later drain into the vascular system.
Drainage implants – Another type of surgery, called
drainage valve implant surgery, may be an option for people with
uncontrolled glaucoma, secondary glaucoma or for children with glaucoma.
A small silicone tube is inserted in the eye to help drain aqueous
fluid.
Treatment for acute angle-closure glaucoma
Acute angle-closure glaucoma is a medical
emergency. Several medications can be used to reduce eye pressure as
quickly as possible. A laser procedure called laser peripheral iridotomy
will also likely be performed. In this procedure, a laser beam creates a
small hole in the iris to allow aqueous fluid to flow more freely into
the front chamber of the eye where it then has access to the meshwork
for drainage.
Lifelong treatment
There is no cure for glaucoma. Patients with
glaucoma need to continue treatment for the rest of their lives. Because
the disease can progress or change silently, compliance with eye
medications and eye examinations are essential, as treatment may need to
be adjusted periodically.
By keeping eye pressure under control, continued
damage to the optic nerve and continued loss of your visual field may
slow or stop. The optometrist may focus on lowering the intraocular
pressure to a level that is least likely to cause further optic nerve
damage. This level is often referred to as the target pressure and will
probably be a range rather than a single number. Target pressure differs
for each person, depending on the extent of the damage and other
factors. Target pressure may change over the course of a lifetime. Newer
medications are always being developed to help in the fight against
glaucoma.
Early detection, prompt treatment and regular
monitoring can help to control glaucoma and therefore reduce the chances
of progression vision loss.
|
Hordeolum
|
See Sty
|
Hyperopia (Farsightedness)
|
See Farsightedness
|
Keratitis
|
An inflammation or infection of the cornea, the
clear front cover of the eye.
|
Keratoconus
|
Keratoconus is a vision disorder that occurs when
the normally round cornea (the front part of the eye) becomes thin and
irregular (cone) shaped. This abnormal shape prevents the light entering
the eye from being focused correctly on the retina and causes distortion
of vision.
In its earliest stages, keratoconus causes slight
blurring and distortion of vision and increased sensitivity to glare and
light. These symptoms usually appear in the late teens or late 20s.
Keratoconus may progress for 10-20 years and then slow in its
progression. Each eye may be affected differently. As keratoconus
progresses, the cornea bulges more and vision may become more distorted.
In a small number of cases, the cornea will swell and cause a sudden and
significant decrease in vision. The swelling occurs when the strain of
the cornea’s protruding cone-like shape causes a tiny crack to develop.
The swelling may last for weeks or months as the crack heals and is
gradually replaced by scar tissue. If this sudden swelling does occur,
your doctor can prescribe eyedrops for temporary relief, but there are
no medicines that can prevent the disorder from progressing.
 Eyeglasses Eyeglasses
or soft contact lenses may be used to correct the mild nearsightedness
and astigmatism that is caused by the early stages for keratoconus. As
the disorder progresses and cornea continues to thin and change shape,
rigid gas permeable contact lenses can be prescribed to correct vision
adequately. In most cases, this is adequate. The contact lenses must be
carefully fitted, and frequent checkups and lens changes may be needed
to achieve and maintain good vision.
In a few cases, a corneal transplant is necessary.
However, even after a corneal transplant, eyeglasses or contact lenses
are often still needed to correct vision.
|
Lazy Eye (Amblyopia)
|
The loss or lack of development of clear vision in
just one eye. It is not due to eye health problems and eyeglasses or
contact lenses can’t fully correct the reduced vision caused by lazy
eye. See also Amblyopia.
|
Learning-related Vision Problems
|
Vision disorders that interfere with reading and
learning.
|
Macular Degeneration
|
Age-Related Macular Degeneration (AMD) is the
leading cause of severe vision loss in adults over age 50. The Centers
for Disease Control and Prevention estimate that 1.8 million people have
AMD and another 7.3 million are at substantial risk for vision loss from
AMD. Caucasians are at higher risk for developing AMD than other races.
Women also develop AMD at an earlier age than men. This eye disease
occurs when there are changes to the macula, a small portion of the
retina that is located on the inside back layer of the eye. AMD is a
loss of central vision that can occur in two forms: “dry” or atrophic
and “wet” or exudative.
Most people with macular degeneration have the dry
form, for which there is no known treatment. The less common wet form
may respond to laser procedures, if diagnosed and treated early.
Some common symptoms are: a gradual loss of ability
to see objects clearly, distorted vision, a gradual loss of color
vision, and a dark or empty area appearing in the center of vision. If
you experience any of these, contact your
doctor of optometry
immediately for a comprehensive examination. Central vision that is lost
to macular degeneration cannot be restored. However, low vision devices,
such as telescopic and microscopic lenses, can be prescribed to maximize
existing vision.
Researchers have linked eye-friendly nutrients such
as lutein/zeaxanthin,
vitamin C,
vitamin E, and
zinc to reducing the risk of
certain eye diseases, including macular degeneration. For more
information on the importance of good nutrition and eye health, please
see the diet and nutrition section.
|
Migraine with Aura
|
See Ocular Migraine
|
Myopia
|
Nearsightedness, or myopia, as it is medically
termed, is a vision condition in which close objects are seen clearly,
but objects farther away appear blurred. Nearsightedness occurs if the
eyeball is too long or the cornea, the clear front cover of the eye, has
too much curvature. As a result, the light entering the eye isn’t
focused correctly and distant objects look blurred.
Nearsightedness is a very common vision condition
affecting nearly 30 percent of the U.S. population. Some research
supports the theory that nearsightedness is hereditary. There is also
growing evidence that it is influenced by the visual stress of too much
close work.
Generally, nearsightedness first occurs in
school-age children. Because the eye continues to grow during childhood,
it typically progresses until about age 20. However, nearsightedness may
also develop in adults due to visual stress or health conditions such as
diabetes.
A common sign of nearsightedness is difficulty with
the clarity of distant objects like a movie or TV screen or the
chalkboard in school. A
comprehensive optometric examination will include testing for
nearsightedness. An optometrist can prescribe eyeglasses or contact
lenses that correct nearsightedness by bending the visual images that
enter the eyes, focusing the images correctly at the back of the eye.
Depending on the amount of nearsightedness, you may only need to wear
glasses or contact lenses for certain activities, like watching a movie
or driving a car. Or, if you are very nearsighted, they may need to be
worn all the time.
Another option for treating nearsightedness is
orthokeratology (ortho-k),
also known as corneal refractive therapy. It is a non-surgical procedure
that involves wearing a series of specially designed rigid contact
lenses to gradually reshape the curvature of your cornea. The lenses
place pressure on the cornea to flatten it. This changes how light
entering the eye is focused.
Laser procedures are also a possible treatment for
nearsightedness in adults. They involve reshaping the cornea by removing
a small amount of eye tissue. This is accomplished by using a highly
focused laser beam on the surface of the eye.
For people with higher levels of nearsightedness,
other refractive
surgery procedures are now available. These procedures involve
implanting a small lens with the desired optical correction directly
inside the eye, either just in front of the natural lens (phakic
intraocular lens implant) or replacing the natural lens (clear lens
extraction with intraocular lens implantation). These procedures are
similar to one used for cataract
surgery patients, who also have lenses implanted in their eyes
(intraocular lens implants).
What causes nearsightedness?

If one or both parents are nearsighted, there is an increased chance
their children will be nearsighted.
The exact cause of nearsightedness is unknown, but
two factors may be primarily responsible for its development:
heredity
visual stress
There is significant evidence that many people
inherit nearsightedness, or at least the tendency to develop
nearsightedness. If one or both parents are nearsighted, there is an
increased chance their children will be nearsighted.
Even though the tendency to develop nearsightedness
may be inherited, its actual development may be affected by how a person
uses his or her eyes. Individuals who spend considerable time reading,
working at a computer, or doing other intense close visual work may be
more likely to develop nearsightedness.
Nearsightedness may also occur due to environmental
factors or other health problems:
Some people may experience blurred distance vision
only at night. This “night myopia” may be due to the low level of light
making it difficult for the eyes to focus properly or the increased
pupil size during dark conditions, allowing more peripheral, unfocused
light rays to enter the eye.
People who do an excessive amount of near vision
work may experience a false or “pseudo” myopia. Their blurred distance
vision is caused by over use of the eyes’ focusing mechanism. After long
periods of near work, their eyes are unable to refocus to see clearly in
the distance. The symptoms are usually temporary and clear distance
vision may return after resting the eyes. However, over time constant
visual stress may lead to a permanent reduction in distance vision.
Symptoms of nearsightedness may also be a sign of
variations in blood sugar levels in persons with
diabetes or an
early indication of a developing
cataract.
An optometrist can evaluate vision and determine
the cause of the vision problems.
How is nearsightedness diagnosed?
Testing for nearsightedness may use several
procedures in order to measure how the eyes focus light and to determine
the power of any optical lenses needed to correct the reduced vision.

A phoropter and retinoscope are often used to determine the lenses that
allow the clearest vision during a comprehensive eye exam.
As part of the testing, letters on a distance chart
are identified. This test measures
visual acuity, which
is written as a fraction such as 20/40. The top number of the fraction
is the standard distance at which testing is performed, twenty feet. The
bottom number is the smallest letter size read. A person with 20/40
visual acuity would have to get within 20 feet to identify a letter that
could be seen clearly at forty feet in a “normal” eye. Normal distance
visual acuity is 20/20, although many people have 20/15 (better) vision.
Using an instrument called a phoropter, an
optometrist places a series of lenses in front of your eyes and measures
how they focus light using a hand held lighted instrument called a
retinoscope. The doctor may choose to use an automated instrument that
automatically evaluates the focusing power of the eye. The power is then
refined by patient’s responses to determine the lenses that allow the
clearest vision.
This testing may be done without the use of eye
drops to determine how the eyes respond under normal seeing conditions.
In some cases, such as for patients who can’t respond verbally, or when
some of the eye’s focusing power may be hidden, eye drops may be used.
They temporarily keep the eyes from changing focus while testing is
performed.
Using the information obtained from these tests,
along with the results of other tests of eye focusing and eye teaming,
your optometrist can determine if you have nearsightedness. He or she
will also determine the power of any lens correction needed to provide
clear vision. Once testing is complete, your optometrist can discuss
options for treatment.
How is nearsightedness treated?
Persons with nearsightedness have several options
available to regain clear distance vision. They include:
eyeglasses
contact lenses
orthokeratology
laser and other refractive surgery procedures
vision therapy for persons with stress-related
nearsightedness.
Eyeglasses are the primary choice of correction for
persons with nearsightedness. Generally, a single vision lens is
prescribed to provide clear vision at all distances. However, for
patients over about age 40, or children and adults whose nearsightedness
is due to the stress of near vision work, a bifocal or progressive
addition lens may be needed. These multifocal lenses provide different
powers or strengths throughout the lens to allow for clear vision in the
distance and also clear vision up close.

Eyeglasses are frequently used to correct myopia.
A large selection of lens types and frame designs
are now available for patients of all ages. Eye glasses are no longer
just a medical device that provides needed vision correction, but can
also be a fashion statement. They are available in a wide variety of
sizes, shapes, colors and materials that not only correct for vision
problems but also may enhance appearance.
For some individuals,
contact lenses can
offer better vision than eyeglasses. They may provide clearer vision and
a wider field of view. However, since contact lenses are worn directly
on the eyes, they require
regular cleaning
and care to safeguard eye health.
Orthokeratology (Ortho-k), also known as corneal refractive therapy,
involves the fitting of a series of rigid contact lenses to reshape the
cornea, the front outer surface of the eye. The contact lenses are worn
daily for limited periods, such as overnight, and then removed. Persons
with moderate amounts of nearsightedness may be able to temporarily
obtain clear vision for most of their daily activities.
Nearsightedness can also be corrected by
reshaping the
cornea using a laser beam of light. Two commonly used procedures are
photorefractive keratectomy (PRK) and laser in situ keratomileusis
(LASIK).
In PRK, a laser is used to remove a thin layer of
tissue from the surface of the cornea in order to change its shape and
refocus light entering the eye. There is a limit to how much tissue can
safely be removed and therefore the amount of nearsightedness that can
be corrected.
LASIK does not remove tissue from the surface of
the cornea, but from its inner layers. To do this, a section of the
outer corneal surface is cut and folded back to expose the inner tissue.
Then a laser is used to remove the precise amount of corneal tissue
needed to reshape the eye, and then the flap of outer tissue is placed
back in position to heal. The amount of nearsightedness that LASIK can
correct is limited by the amount of corneal tissue that can be removed
in a safe manner.
People who are highly nearsighted or whose corneas
are too thin to allow the use of laser procedures now have another
option. They may be able to have their nearsightedness surgically
corrected by implanting small lenses in their eyes. These intraocular
lenses look like small contact lenses and they provide the needed
optical correction directly inside the eye.
Vision therapy is an option for people whose
blurred distance vision is caused by a spasm of the muscles which
control eye focusing. Various eye exercises can be used to improve poor
eye focusing ability and regain clear distance vision.
People with nearsightedness have a variety of
options to correct their vision problem. In consultation with your
optometrist, you can select the treatment that best meets you visual and
lifestyle needs.
|
Nearsightedness
|
A vision condition in which you can see close
objects clearly, but objects farther away are blurred.
|
Nystagmus
|
Nystagmus is a vision condition in which the eyes
make repetitive, uncontrolled movements, often resulting in reduced
vision. These involuntary eye movements can occur from side to side, up
and down, or in a circular pattern. As a result, both eyes are unable to
hold steady on objects being viewed. Nystagmus may be accompanied by
unusual head positions and head nodding in an attempt to compensate for
the condition.
Nystagmus can be inherited and appear in early
childhood or develop later in life due to an accident or illness.
Generally, nystagmus is a symptom of some other underlying eye or
medical problem. However, the exact cause is often unknown.
Persons with nystagmus may experience reduced
visual acuity. They may also have problems with depth perception that
can affect their balance and coordination. Nystagmus can be aggravated
by fatigue and stress.
Most individuals with nystagmus can reduce the
severity of their uncontrolled eye movements and improve vision by
positioning their eyes to look to one side. This is called the “null
point” where the least amount of nystagmus is evident. To accomplish
this they may need to adopt a specific head posture to make the best use
of their vision.
The forms of nystagmus include:
Congenital – most often develops by 2 to 3 months
of age. The eyes tend to move in a horizontal swinging fashion. It is
often associated with other conditions such as albinism, congenital
absence of the iris (the colored part of the eye), underdeveloped optic
nerves, and congenital cataract.
Spasmus nutans – usually occurs between 6 months
and 3 years of age and resolves spontaneously between 2 and 8 years of
age. Children with this form of nystagmus often display head nodding and
a head tilt. Their eyes may move in any direction. This type of
nystagmus usually does not require treatment.
Acquired – develops later in childhood or
adulthood. The cause is often unknown, but it may be due to central
nervous system and metabolic disorders or alcohol and drug toxicity.
Nystagmus can be further classified by the type of
motion the eyes make:
Pendular nystagmus – the speed of movement of the
eyes is in same in both directions.
Jerk nystagmus – the eyes move slowly in one
direction and then quickly “jerk” back in the other direction.
What causes nystagmus?
Nystagmus results from the instability or
impairment of the system responsible for controlling eye movements. When
nystagmus develops in early childhood, it can be caused by a problem
with the visual pathway from the eye to the brain. Often the child has
no other eye or medical problem. Acquired nystagmus, which occurs later
in life, can be the symptom of another condition such as stroke,
multiple sclerosis or a blow to the head.
Other causes of nystagmus include:
Lack of development of normal eye movement control
early in life
Albinism
Very high refractive error, e.g. nearsightedness
(myopia) or astigmatism
Congenital cataracts
Inflammation of the inner ear
Medications such as anti-epilepsy drugs
Central nervous system diseases
How is nystagmus diagnosed?
Nystagmus can be diagnosed through a comprehensive
eye exam. Testing for nystagmus, with special emphasis on how the eyes
move, may include:
Patient history to determine any symptoms the
patient is experiencing and the presence of any general health problems,
medications taken, or environmental factors that may be contributing to
the symptoms.
Visual acuity measurements to assess the extent to
which vision may be affected.
A refraction to determine the appropriate lens
power needed to compensate for any refractive error (nearsightedness,
farsightedness, or astigmatism).
Testing how the eyes focus, move and work together.
In order to obtain a clear, single image of what is being viewed, the
eyes must effectively change focus, move and work in unison. This
testing will look for problems that affect the control of eye movements
or make it difficult to use both eyes together.
Since nystagmus is often the result of other
underlying health problems, your optometrist may refer you to your
primary care physician or other medical specialist for further testing.
Using the information obtained from testing, your
optometrist can determine if you have nystagmus and advise you on
treatment options.
How is nystagmus treated?
Nystagmus can not be cured. While eyeglasses and
contact lenses do not correct nystagmus, they can help to correct other
vision problems such as nearsightedness, farsightedness or astigmatism.
Some types of nystagmus improve throughout
childhood. In addition, vision may be enhanced with prisms and special
glasses. The use of large-print books, magnifying devices and increased
lighting can also be helpful.
Rarely, surgery is performed to alter the position
of the muscles, which move the eyes. While it does not cure nystagmus,
it may reduce the amount of head turn needed for best vision.
Treatment for other underlying eye or medical
problems may help to improve or reduce nystagmus.
|
Ocular Allergies
|
The abnormal response of sensitive eyes to contact
with allergens and other irritating substances.
|
Ocular Hypertension
|
Ocular hypertension is an increase in the pressure
in your eyes that is above the range considered normal with no
detectable changes in vision or damage to the structure of your eyes.
The term is used to distinguish people with elevated pressure from those
with glaucoma, a serious eye disease that causes damage to the optic
nerve and vision loss.
Ocular hypertension can occur in people of all
ages, but it occurs more frequently in African Americans, those over age
40 and those with family histories of ocular hypertension and/or
glaucoma. It is also more common in those who are very nearsighted or
who have diabetes.
Ocular hypertension has no noticeable signs or
symptoms. Your doctor of optometry can check the pressure in your eyes
with an instrument called a tonometer and can examine the inner
structures of your eyes to assess your overall eye health.
Not all people with ocular hypertension will
develop glaucoma. However, there is an increased risk of glaucoma among
those with ocular hypertension, so regular comprehensive optometric
examinations are essential to your overall eye health.
There is no cure for ocular hypertension, however,
careful monitoring and treatment, when indicated, can decrease the risk
of damage to your eyes.
|
Ocular Migraine
|
A type of severe headache accompanied by various
visual symptoms.
|
Pinquecula
|
An abnormal growth of tissue on the conjunctiva,
the clear membrane that covers the white of the eye.
|
Presbyopia
|
Presbyopia is a vision condition in which the
crystalline lens of your eye loses its flexibility, which makes it
difficult for you to focus on close objects.
Presbyopia may seem to occur suddenly, but the
actual loss of flexibility takes place over a number of years.
Presbyopia usually becomes noticeable in the early to mid-40s.
Presbyopia is a natural part of the aging process of the eye. It is not
a disease, and it cannot be prevented.
Some signs of presbyopia include the tendency to
hold reading materials at arm’s length, blurred vision at normal reading
distance and eye fatigue along with headaches when doing close work. A
comprehensive optometric examination will include testing for
presbyopia.
To help you compensate for presbyopia, your
optometrist can prescribe reading glasses, bifocals, trifocals or
contact lenses. Because presbyopia can complicate other common vision
conditions like nearsightedness, farsightedness and astigmatism, your
optometrist will determine the specific lenses to allow you to see
clearly and comfortably. You may only need to wear your glasses for
close work like reading, but you may find that wearing them all the time
is more convenient and beneficial for your vision needs.
Because the effects of presbyopia continue to
change the ability of the crystalline lens to focus properly, periodic
changes in your eyewear may be necessary to maintain clear and
comfortable vision.
|
Pterygium
|
An abnormal growth of tissue on the conjuctiva, the
clear membrane that covers the white of the eye, and the adjacent
cornea, the clear front surface of the eye.
|
Ptosis
|
A drooping of the upper eyelid.
|
Retinal Detachment
|
A tearing or separation of the retina, the light
sensitive lining at the back of the eye, from the underlying tissue.
|
Retinitis Pigmentosa
|

The first sign of retinitis pigmentosa is often night blindness followed
by a slow loss of side vision.
Retinitis pigmentosa (RP) is a group of inherited
diseases that damage the light-sensitive rods and cones located in the
retina, the back part of our eyes. Rods, which provide side (peripheral)
and night vision are affected more than the cones that provide color and
clear central vision.
Signs of RP usually appear during childhood or
adolescence. The first sign is often night blindness followed by a slow
loss of side vision. Over the years, the disease will cause further loss
of side vision. As the disease develops, people with RP may often bump
into chairs and other objects as side vision worsens and they only see
in one direction – straight ahead. They see as if they are in a tunnel
(thus the term tunnel vision).
Fortunately, most cases of retinitis pigmentosa
take a long time to develop and vision loss is gradual. It may take many
years for loss of vision to be severe.
Currently, there is no cure for RP, but there is
research that indicates that vitamin A and lutein may slow the rate at
which the disease progresses. Your doctor of optometry can give you more
specific information on nutritional supplements that may help you.
Also, there are many new low vision aids, including
telescopic and magnifying lenses, night vision scopes as well as other
adaptive devices, that are available that help people maximize the
vision that they have remaining. An optometrist, experienced in low
vision rehabilitation, can provide these devices as well as advice about
other training and assistance to help people remain independent and
productive.
Becuase it is an inherited disease, research into
genetics may one day provide a prevention or cure for those who have RP.
|
Retinoblastoma
|
Every parent dreads to hear the word “cancer,” but
cancer has a high prevalence in the United States. Early detection of
cancer can greatly reduce the severity of the illness and increase life
expectancy.
Optometrists diagnose, refer, and comanage cancers
that involve the eye area. The most common cancer involving the eye in
young children is retinoblastoma. In the United States, this
fast-growing cancer occurs in 1 in every 20,000 children, making it the
tenth most common pediatric cancer.
There are 2 forms of retinoblastoma—hereditary and
sporadic. Although sporadic retinoblastoma occurs more frequently,
families with a history of hereditary retinoblastoma should be assessed.
Adapted from Hoppe E, Frankel R. Optometrists as
key providers in the prevention and early detection of malignancies.
Optometry (2006) 77, 397-404
|
Strabismus
|
Crossed eyes, or strabismus as it is medically
termed, is a condition in which both eyes do not look at the same place
at the same time. It occurs when an eye turns in, out, up or down and is
usually caused by poor eye muscle control or a high amount of
farsightedness.
There are six muscles attached to each eye that
control how it moves. The muscles receive signals from the brain that
direct their movements. Normally, the eyes work together so they both
point at the same place. When problems develop with eye movement
control, an eye may turn in, out, up or down. The eye turning may be
evident all the time or may appear only at certain times such as when
the person is tired, ill, or has done a lot of reading or close work. In
some cases, the same eye may turn each time, while in other cases, the
eyes may alternate turning.
Maintaining proper eye alignment is important to
avoid seeing double, for good depth perception, and to prevent the
development of poor vision in the turned eye. When the eyes are
misaligned, the brain receives two different images. At first, this may
create double vision and confusion, but over time the brain will learn
to ignore the image from the turned eye. If the eye turning becomes
constant and is not treated, it can lead to permanent reduction of
vision in one eye, a condition called amblyopia or lazy eye.
Some babies’ eyes may appear to be misaligned, but
are actually both aiming at the same object. This is a condition called
pseudostrabismus or false strabismus. The appearance of crossed eyes may
be due to extra skin that covers the inner corner of the eyes, or a wide
bridge of the nose. Usually, this will change as the child’s face begins
to grow.
Strabismus usually develops in infants and young
children, most often by age 3, but older children and adults can also
develop the condition. There is a common misconception that a child with
strabismus will outgrow the condition. However, this is not true. In
fact, strabismus may get worse without treatment. Any child older than
four months whose eyes do not appear to be straight all the time should
be examined.
Strabismus is classified by the direction the eye
turns:
Inward turning is called esotropia
Outward turning is called exotropia
Upward turning is called hypertropia
Downward turning is called hypotropia.
Other classifications of strabismus include:
The frequency with which it occurs – either
constant or intermittent
Whether it always involves the same eye –
unilateral
If the turning eye is sometimes the right eye and
other times the left eye – alternating.
Treatment for strabismus may include eyeglasses,
prisms, vision therapy, or eye muscle surgery. If detected and treated
early, strabismus can often be corrected with excellent results.[
What causes strabismus?
Strabismus can be caused by problems with the eye
muscles, the nerves that transmit information to the muscles, or the
control center in the brain that directs eye movements. It can also
develop due to other general health conditions or eye injuries.
Risk factors for developing strabismus include:
Family history – individuals with parents or
siblings who have strabismus are more likely to develop it.
Refractive error – people who have a significant
amount of uncorrected farsightedness (hyperopia) may develop strabismus
because of the additional amount of eye focusing required to keep
objects clear.
Medical conditions – people with conditions such as
Down syndrome and cerebral palsy or who have suffered a stroke or head
injury are at a higher risk for developing strabismus.
Although there are many types of strabismus that
can develop in children or adults, the two most common forms are
accommodative esotropia and intermittent exotropia.
Accommodative esotropia often occurs because of
uncorrected farsightedness (hyperopia). Because the eye’s focusing
system is linked to the system that controls where the eyes point, the
extra focusing effort needed to keep images clear in farsightedness may
cause the eyes to turn inward. Signs and symptoms of accommodative
esotropia may include seeing double, closing or covering one eye when
doing close work, and tilting or turning of the head.
Intermittent exotropia may develop due to an
inability to coordinate both eyes together. The eyes may have a tendency
to point beyond the object being viewed. People with intermittent
exotropia may experience headaches, difficulty reading, and eye strain.
They also may have a tendency to close one eye when viewing at distance
or in bright sunlight.
How is strabismus diagnosed?
Strabismus is diagnosed through a comprehensive eye
exam. Testing for strabismus, with special emphasis on how the eyes
focus and move, may include:
Patient History – A patient history is obtained to
determine any symptoms the patient is experiencing or the parent is
observing, and to note the presence of any general health problems,
medications taken, or environmental factors that may be contributing to
the symptoms.
Visual Acuity – Visual acuity measurements are
taken to assess the extent to which vision may be affected. As part of
the testing, you will be asked to read letters on distance and near
reading charts. This test measures visual acuity, which is written as a
fraction such as 20/40. When testing distance vision, the top number is
the standard distance at which testing is done, twenty feet. The bottom
number is the smallest letter size you were able to read at the twenty
foot distance. A person with 20/40 visual acuity would have to get
within 20 feet of a letter that should be seen at forty feet in order to
see it clearly. “Normal” distance visual acuity is 20/20.
Refraction – A refraction is conducted to determine
the appropriate lens power needed to compensate for any refractive error
(nearsightedness, farsightedness, or astigmatism). Using an instrument
called a phoropter, your optometrist places a series of lenses in front
of your eyes and measures how they focus light using a hand held lighted
instrument called a retinoscope. Or the doctor may choose to use an
automated instrument that automatically evaluates the refractive power
of the eye. The power is then refined by the patient’s responses to
determine the lenses that allow the clearest vision.
Alignment and Focusing Testing – How well your eyes
focus, move and work together needs to be assessed. In order to obtain a
clear, single image of what is being viewed, the eyes must effectively
change focus, move and work in unison. This testing will look for
problems that keep your eyes from focusing effectively or make it
difficult to use both eyes together.
Examination of eye health – The structures of the
eye are observed to rule out any eye disease that may be contributing to
strabismus. The health of the external and internal parts of the eye
will be assessed using various testing procedures.
This testing may be done without the use of eye
drops to determine how the eyes respond under normal seeing conditions.
In some cases, such as for patients who can’t respond verbally or when
some of the eyes focusing power may be hidden, eye drops may be used.
They temporarily keep the eyes from changing focus while testing is
done.
Using the information obtained from these tests,
along with results of other tests, your optometrist can determine if you
have strabismus. Once testing is complete, your optometrist can discuss
options for treatment.
How is strabismus treated?
People with strabismus have several treatment
options available to improve eye alignment and coordination. They
include:
eyeglasses or contact lenses
prism lenses
vision therapy
eye muscle surgery
Eyeglasses or contact lenses may be prescribed for
patients with uncorrected farsightedness. This may be the only treatment
needed for some patients with accommodative esotropia. Once the
farsightedness is corrected, the eyes require less focusing effort and
may remain straight.
Prism lenses are special lenses that have a
prescription for prism power in them. The prisms alter the light
entering the eye and assist in reducing the amount of turning the eye
has to do to look at objects. Sometimes the prisms are able to fully
compensate for and eliminate the eye turning.
Vision therapy is a structured program of visual
activities prescribed to improve eye coordination and eye focusing
abilities. Vision therapy trains the eyes and brain to work together
more effectively. These eye exercises help remediate deficiencies in eye
movement, eye focusing and eye teaming and reinforce the eye-brain
connection. Treatment may include office-based as well as home training
procedures.
Eye muscle surgery can change the length or
position of the muscles around the eye in an attempt to better align the
eyes. Eye muscle surgery may be able to physically align the eyes so
they appear straight. Often a program of vision therapy may also be
needed to develop a functional improvement in eye coordination and to
keep the eyes from reverting back to their previous condition of
misalignment.
Also See Crossed Eyes.
|
Sty
|
An infection of an oil gland in the eyelid.
|
Subconjunctival Hemorrhage
|
An accumulation of blood underneath the
conjunctiva, the clear membrane covering the white part of the eye.
|
Uveitis
|
Anterior uveitis is an inflammation of the middle
layer of the eye, which includes the iris (colored part of the eye) and
adjacent tissue, known as the ciliary body. If untreated, it can cause
permanent damage and loss of vision from the development of glaucoma,
cataract or retinal edema. It usually responds well to treatment;
however, there may be a tendency for the condition to recur. Treatment
usually includes prescription eye drops, which dilate the pupils, in
combination with anti-inflammatory drugs. Treatment usually takes
several days, or up to several weeks, in some cases.
Anterior uveitis can occur as a result of trauma to
the eye, such as a blow or foreign body penetrating the eye. It can also
be a complication of other eye disease, or it may be associated with
general health problems such as rheumatoid arthritis, rubella and mumps.
In most cases, there is no obvious underlying cause.
Signs/symptoms may include a red, sore and inflamed
eye, blurring of vision, sensitivity to light and a small pupil. Becuase
the symptoms of anterior uveitis are similar to those of other eye
diseases, your optometrist will carefully examine the inside of your
eye, under bright light and high magnification, to determine the
presence and severity of the condition. Your optometrist may also
perform or arrange for other diagnostic tests to help pinpoint the
cause.
Some symptoms of Anterior uveitis include a red, sore and inflamed eye,
and a small pupil.
|




 Eyeglasses are a common form of correction for persons with astigmatism.
Eyeglasses are a common form of correction for persons with astigmatism. Blepharitis can appear as greasy flakes or scales around the base of the
Blepharitis can appear as greasy flakes or scales around the base of the



 Red-green deficiency results in the inability to distinguish certain
Red-green deficiency results in the inability to distinguish certain



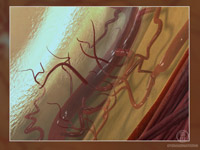

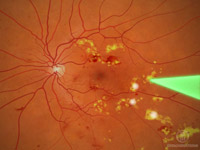
 Poor
Poor



 Eyeglasses
Eyeglasses